Helping Our Children: Supporting Their Mental Health
January 12, 2022WHAT ARE THE SIGNS OF A MENTAL HEALTH CRISIS?
Learn the signs to look for that you or someone you know might be experiencing a mental health crisis and learn how to access the help needed through support and treatment.
First, let’s be aware of the challenges facing our kids, which could precipitate a crisis. This is not an all- inclusive list, and mental health challenges could also seemingly appear out of the blue.
The Challenges…
- The COVID-19 Pandemic/Quarantine - Isolation, lack of socialization, changes in routine, and facing the reality of death from Covid can all contribute to anxiety and depression
- Economic/Financial Issues - If your family is facing these challenges, your children are feeling them, too.
- The Racial Divide - The world’s concerns often become our children’s concerns. Children often have a fine-tuned sense of justice, and challenges to their internal compass for justice often results in anxiety.
- Politics/Election - It was stressful for all of us!
- Violence - Children are struggling to make sense of the violence they see in the news, and any familial violence is traumatic to all involved.
- Learning Remotely/Working Remotely - Changes in routine can greatly disrupt a child’s world
- Natural Disasters/Weather Events - Uncontrollable events are often a source of anxiety
- Constant Exposure through News and Social Media - It’s affecting us as adults, just imagine what it does to our children who lack the maturity to keep it all in context
- Grief and Loss - This applies not only to illness and death of loved ones, but there is also a sense of grief and loss for their pre-pandemic lives.
SO, WHAT CONSTITUTES A CRISIS?
A crisis situation can be anything which you need help to handle. Being in crisis is NOT a sign of bad parenting, in fact, it may be the opposite. Recognizing that you need help to help your child is selfless, and an act of good parenting!
CRISIS SITUATION: YOUR ROLE

Types of Crisis Situations
- Medical emergency
- Panic attack
- Aggressive behaviours
- Substance use
- Traumatic event
- Non-suicidal self-injury
- Severe psychotic states
- Suicidal thoughts
Signs and Symptoms of a Crisis Situation: Medical Emergencies
- Unintentionally throwing up several times a day
- Fainting
- Collapsing or being too weak to walk
- Painful muscle spasms
- Chest pain or difficulty breathing
- Blood in bowel movements, urine, or vomit
- An irregular or very low heartbeat or respiratory rate
- Cold or clammy skin indicating a low body temperature
Signs and Symptoms of a Crisis Situation: Psychosis
- Social isolation or withdrawal
- Difficulty concentrating or paying attention
- Decreased work or school performance
- Decline in self-care or personal hygiene
- Changes in appetite
- Unusual sleep disturbances
- Dressing inappropriately for the weather
- Showing limited, flat, or inappropriate emotions or facial expressions
- Confused or disorganized manner of speech
- Suspicion or expressing unusual, intense new, or odd ideas
- Voicing strange feelings
- Delusions or hallucinations
Signs and Symptoms of a Crisis Situation: Warning Signs of Suicidal Thoughts
- Talking or writing about death, dying, or suicide
- Threatening to hurt or kill themselves
- Looking for ways to kill themselves, seeking access to means
- Showing anxiety or agitation
- Being unable to sleep or sleeping all the time
- Feeling no reason for living, no sense of purpose in life
- Feeling trapped, like there is no way out
- Thinking there is no reason for living
- Thinking there is no safe way out of a bad situation
HOW TO DEESCALATE
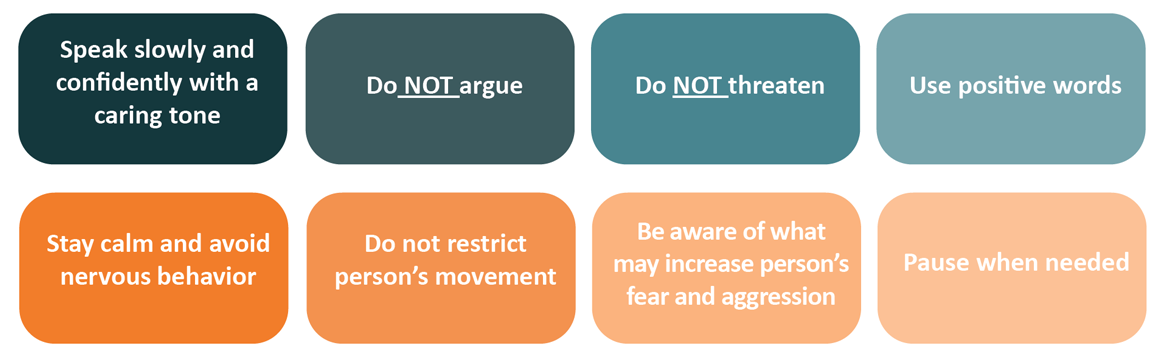
CRISIS SITUATIONS: SAFETY CONSIDERATIONS

IS THIS JUST A STAGE?
Now you know why these changes may happen, let’s talk about concrete things to look for which should trigger you to seek an evaluation from a pediatrician or mental health professional.
- Always seek immediate help if a child engages in unsafe behavior or talks about wanting to hurt him or herself or someone else.
- Seek help when a child’s behavior or emotional difficulties last for more than a few weeks and are causing problems at school, at home, or with friends.
- A thorough evaluation can help determine if treatment is necessary, and which treatments may be most effective.
- Early treatment can help address a child’s current difficulties and can also help prevent more serious problems in the future.

WHEN TO SEEK HELP
Even under the best of circumstances, it can be hard to tell the difference between challenging behaviors and emotions that are consistent with typical child development and those that are cause for concern. It is important to remember that many disorders like anxiety, attention deficit hyperactivity disorder and depression, do occur during childhood. In fact, many adults who seek treatment reflect back on how these disorders affected their childhood and wish that they had received help sooner. In general, if a child’s behavior persists for a few weeks or longer, causes distress for the child or the child’s family, and interferes with functioning at school, at home, or with friends, then consider seeking help. If a child’s behavior is unsafe, or if a child talks about wanting to hurt him or herself or someone else, then seek help immediately.
Young children may benefit from an evaluation and treatment if they:
- Have frequent tantrums or are intensely irritable much of the time
- Often talk about fears or worries
- Complain about frequent stomach aches or headaches with no known medical cause
- Are in constant motion and cannot sit quietly (except when they are watching videos or playing video games)
- Sleep too much or too little, have frequent nightmares, or seem sleepy during the day
- Are not interested in playing with other children or have difficulty making friends
- Struggle academically or have experienced a recent decline in grades
- Repeat actions or check things many times out of fear that something bad may happen.
Older children and adolescents may benefit from an evaluation if they:
- Have lost interest in things that they used to enjoy
- Have low energy
- Sleep too much or too little, or seem sleepy throughout the day
- Are spending more and more time alone, and avoid social activities with friends or family
- Fear gaining weight, or diet or exercise excessively
- Engage in self-harm behaviors (e.g., cutting or burning their skin)
- Smoke, drink, or use drugs
- Engage in risky or destructive behavior alone or with friends
- Have thoughts of suicide
- Have periods of highly elevated energy and activity, and require much less sleep than usual
- Say that they think someone is trying to control their mind or that they hear things that other people cannot hear.

I’VE DECIDED MY CHILD SHOULD BE EVALUATED. WHERE DO I GO, WHAT DO I DO?
First, if your child is actively harming themselves, having suicidal thoughts, or planning to hurt others, call 2-1-1 and press option 1 for the Mobile Crisis Service. This is a 24 hour, 7 day a week free service to have your child immediately evaluated by a mental health professional. NOTE: If calling by cell phone, 2-1-1 can also be reached toll-free at: 800-203-1234
WHAT TO EXPECT AFTER YOU CALL 2-1-1 - A social worker or other mental health professional will arrive within 45 minutes most times, and will come in a discreet vehicle, unless an ambulance is needed or a 911 phone call is made. The social worker will speak directly with the child to assess any immediate risk, and then make recommendations to the parent for further evaluation, treatment, or other options.
PLEASE NOTE - There is no shame in having the Emergency Mobile Crisis team to come to your home. Every professional on the team would rather you err on the side of caution. If you feel you should call, then call. Trust your gut. Do not have any concerns about overreacting, placing any burdens on others by calling, or fear any stigma associated with calling for the service. The service is confidential, it is not listed in the police blotter, there is no fee. This service is available for exactly this reason - to help a child and family in crisis.

IF YOUR CHILD IS NOT IN CRISIS, BUT YOU HAVE CONCERNS ABOUT YOUR CHILD’S MENTAL WELL-BEING, HERE’S HOW YOU CAN BEGIN
First Steps for Parents
- Talk with your child’s teacher. What is the child’s behavior like in school, daycare, or on the playground?
- Talk with your child’s pediatrician. Describe the behavior, and report what you have observed and learned from talking with others.
- Ask for a referral to a mental health professional who has experience and expertise dealing with children.
Finding Answers
- An evaluation by a health professional can help clarify problems that may be underlying a child’s behavior and provide reassurance or recommendations for next steps.
- It provides an opportunity to learn about a child’s strengths and weaknesses and determine which interventions might be most helpful.
A comprehensive assessment of a child’s mental health includes the following:
- An interview with parents addressing a child’s developmental history, temperament, relationships with friends and family, medical history, interests, abilities, and any prior treatment. It is important to get a picture of the child’s current situation, for example: has he or she changed schools recently, has there been an illness in the family, or a change with an impact on the child’s daily life.
- Information gathering from school, such as standardized tests, reports on behavior, capabilities, and difficulties.
- An interview with the child about his or her experiences, as well as testing and behavioral observations, if needed.
TREATMENT OPTIONS
- Assessment results may suggest that a child’s behavior is related to changes or stresses at home or school; or is the result of a disorder for which treatment would be recommended. Treatment recommendations may include:
- Psychotherapy (“talk therapy”). There are many different approaches to psychotherapy, including structured psychotherapies directed at specific conditions.
- Information about types of psychotherapies is available on the National Institute of Mental Health (NIMH) Psychotherapies page. Effective psychotherapy for children always includes:
- Parent involvement in the treatment (especially for children and adolescents)
- Teaching skills and practicing skills at home or at school (between session “homework assignments”)
- Measures of progress (e.g., rating scales, improvements on homework assignments) that are tracked over time.
- Medications. Medication may be used along with psychotherapy. As with adults, the type of medications used for children depends on the diagnosis and may include antidepressants, stimulants, mood stabilizers, and others. General information on specific classes of medications is available on NIMH’s mental health medications page. Medications are often used in combination with psychotherapy. If different specialists are involved, treatment should be coordinated.
- Family counseling. Including parents and other members of the family in treatment can help families understand how a child’s individual challenges may affect relationships with parents and siblings and vice versa.
- Support for parents. Individual or group sessions that include training and the opportunity to talk with other parents can provide new strategies for supporting a child and managing difficult behavior in a positive way. The therapist can also coach parents on how to deal with schools.
- To find information about treatment options for specific disorders, visit www.nimh.nih.gov/health/.
CHOOSING A MENTAL HEALTH PROFESSIONAL
It’s especially important to look for a child mental health professional who has training and experience treating the specific problems that your child is experiencing. Ask the following questions when meeting with prospective treatment providers:
- Do you use treatment approaches that are supported by research?
- Do you involve parents in the treatment? If so, how are parents involved?
- Will there be homework between sessions?
- How will progress from treatment be evaluated?
- How soon can we expect to see progress?
- How long should treatment last?

FOR PARENTS: WHAT’S NEXT?
You’ve gotten the ball rolling on finding help for your child, but what should you do to support your child’s mental health at home and school?
First, be active in your child’s treatment. Ask your clinician what changes should be made at home to support your child’s treatment.
Educate yourself. NAMI: National Alliance on Mental Illness provides wonderful courses for parents and children. NAMI Basics OnDemand is a free, six-session online education program for parents, caregivers and other family who provide care for youth aged 22 or younger who are experiencing mental health symptoms. NAMI Basics OnDemand is an adaptation of the in-person course offered in 43 states by NAMI affiliates. It is a must-attend for parents and caregivers, and can be done on-demand, at your pace.
Try a Little Tenderness. Thinking of your child’s depression or anxiety as an illness will help remind you that it’s not something they can just “get over”, or “toughen up” about, just like they can’t just “power through” diabetes or broken bones. Recovering from mental illness requires treatment, sometimes it requires medication, and it isn’t solved overnight. Prepare yourself for a longer term recovery, and be committed to finding the right accommodations and home structure for your child. It won’t be perfect, recovery isn’t linear. But a little understanding goes a long way.
Don’t forget to take care of yourself. Parenting a child with a mental illness isn’t easy, but the work is worth it. However, you can’t help anyone if you’re suffering yourself.
Consider this your permission to seek counseling on your own to help you through this difficult time. Family counseling can help everyone come together for a harmonious home.
CHILD IN CRISIS: QUICK ACTION GUIDE
- Call 2-1-1 from a landline; when prompted follow 1-1 again. All 211 calls are screened for a police or ambulance. Only dial 911 if it’s a medical emergency.
- Call the National Suicide Prevention Lifeline (Lifeline) at 1-800-273-TALK (8255)
- Text the Crisis Text Line (text HELLO to 741741) - Available 24/7, 365 days a year, this organization helps people with mental health challenges by connecting callers with trained crisis volunteers who will provide confidential advice, support, and referrals if needed.
- Lifeline Chat - chat online with crisis centers around the United States.
- The Trevor Project (Call 866-488-7386 or Text “START” to 678678) - Trained counselors available 24/7 to support youth who are in crisis, feeling suicidal, or in need of a safe and judgment free place to talk. Specializing in supporting the LGBTQI+ community.
Help Lines
- Disaster Distress Helpline: 1-800-985-5990 (press 2 for Spanish), or text TalkWithUs for English or Hablanos for Spanish to 66746. Spanish speakers from Puerto Rico can text Hablanos to 1-787-339-2663.
- National Suicide Prevention Lifeline: 1-800-273-TALK (8255) for English, 1-888-628-9454 for Spanish, or Lifeline Crisis Chat.
- National Domestic Violence Hotline: 1-800-799-7233 or text LOVEIS to 22522
- National Child Abuse Hotline: 1-800-4AChild (1-800-422-4453) or text 1-800-422-4453
- National Sexual Assault Hotline: 1-800-656-HOPE (4673) or Online Chat
- The Eldercare Locator: 1-800-677-1116
- Veteran’s Crisis Line: 1-800-273-TALK (8255) or Crisis Chat or text: 8388255
- Youth or Young Crisis Text Line - Text “LISTEN” to 741-741, or visit http://www.crisistextline.org/ for more info.
If your child is actively harming themselves, having suicidal thoughts, or planning to hurt others, call 911, or 2-1-1 and press option 1 for the Mobile Crisis Service. This is a 24 hour, 7 day a week free service to have your child immediately evaluated by a mental health professional. NOTE: If calling by cell phone, 2-1-1 can also be reached toll-free at: 800.203.1234
WHAT TO EXPECT AFTER YOU CALL 2-1-1 - A social worker or other mental health professional will arrive within 45 minutes most times, and will come in a discreet vehicle, unless an ambulance is needed or a 911 phone call is made. The social worker will speak directly with the child to assess any immediate risk, and then make recommendations to the parent for further evaluation, treatment, or other options.

CTC RESOURCES FOR CHILDREN AND ADOLESCENTS
Provided by Connecting to Care CT
DESCRIPTION OF SERVICES
 |
CARE COORDINATION System Navigation Care Coordinators work with families to identify their needs, navigate and link to supports and services, coordinate their care and advocate for their needs. |
 |
MOBILE CRISIS Crisis Stabilization Centralized, toll-free number (2-1-1) for person-to-person assistance and connection to local crisis services; accessible 24/7, 365 days a year. Caller defines crisis & setting. |
 |
OUTPATIENT PSYCHIATRIC CLINICS FOR CHILDREN (OPCC) Outpatient Treatment Community-based, multi-disciplinary team of psychiatrists, psychologists, clinicians and other professionals that provide a wide array of behavioral health treatment services to children, adolescents and their families. |
*If you or someone you know is experiencing a crisis, access Mobile Crisis directly by dialing 2-1-1 and then enter 1, 1 when prompted.
REGIONAL SERVICES – CENTRAL
| Name of Agency | Service Provided | Location | Contact |
|---|---|---|---|
| Child Guidance Clinic of Central CT | Outpatient Services | 384 Pratt Street Meriden, CT 06450 |
(203) 235-5767 |
| Community Mental Health Affiliates | Outpatient Services | 233 Main Street New Britain, CT 06051 |
(860) 826-1358 |
| Wheeler Clinic | Outpatient Services Mobile Crisis* Care Coordination |
91 Northwest Drive Plainville, CT 06062 |
(860) 793-3567 |
| Rushford Center Inc. | Care Coordination | 883 Paddock Avenue Meriden, CT 06450 |
(203) 634-7061 |
*Wheeler Clinic serves as the provider for Mobile Crisis services that are accessible through 2-1-1.
REGIONAL SERVICES – WESTERN
| Name of Agency | Service Provided | Location | Contact |
|---|---|---|---|
| Community Mental Health Affiliates | Outpatient Services | 36 Sheffield Street Waterbury, CT |
(860) 826-1358 |
| Wellmore, Inc. | Outpatient Services Care Coordination |
70 Pine Street Waterbury, CT 06710 |
(203) 575-0466 ext. 115 |
| Wellmore, Inc. | Outpatient Services Care Coordination |
150 Meadow Street Naugatuck, CT 06770 |
(203) 575-0466 ext. 115 |
| Wellmore, Inc. | Care Coordination Mobile Crisis* |
402 E. Main Street Waterbury, CT 06702 |
(203) 755-1143 |
*Wellmore serves as the provider for Mobile Crisis services that are accessible through 2-1-1.
REGIONAL YSBs
14 Youth Service Bureaus serve 14 towns in the Central Region
Cheshire Youth & Social Services, Inc.
84 South Main Street
Cheshire, CT 06410
(203) 271-6690
Meriden Youth Services
165 Miller Street
Meriden, CT 06450
(203) 630-4221
For more information or to find another YSB, visit: https://www.ctyouthservices.org.
CONTACT US!
For questions, additional information, or connection to services, please contact:
| CENTRAL REGION | WESTERN REGION |
|---|---|
| Kenisha Creary Network of Care Manager for Central Region 6 kenisha.creary@beaconhealthoptions.com 860-637-9062 |
Julie Calabro Network of Care Manager for Southwest Region 5 julie.calabro@beaconhealthoptions.com 860-263-2437 |
| Stan Kasanowski System Program Director for Region 6 stanley.kasanowski@ct.gov 860-221-5966 |
Sergio Alvarez System Program Director for Region 5 sergio.alvarez@ct.gov 860-209-1083 |

FOR THOSE TIMES YOU NEED TO TALK IT OUT
ANXIETY. EMPTINESS. SADNESS.
One conversation can make all the difference in the world. It just takes a simple text.
- Text talk to 38255
You’ll immediately be put into contact with a master’s-level counselor.
- Get connected
As they get started, they’ll ask for your birthdate and ZIP code. Although you don’t have to answer, this info helps them help others.
- Start a conversation
Then they’ll just text about what’s going on. No issue is too small or too great.

Southwest Region Resource List
Updated 10.22.21
For Mobile Crisis, dial 2-1-1, press “1” and “1” again to be directly connected
| Community Based Behavioral Health |
LEGEND | Outpatient Psychiatric Clinics for Children (OPCC) | Extended Day Treatment (EDT) | Care Coordination (CC) | Mobile Crisis (MC) |Modular Approach to Therapy for Children (MATCH) |
Trauma-Focused Cognitive Behavioral Therapy (TF-CBT)
For mobile crisis, dial 2-1-1, press “1” and “1” again to be directly connected
| Name of Agency | Service Provided | Location | Contact |
| Boys and Girls Village | OPCC/EDT TF-CBT |
528 Wheeler Farms Road Milford, CT 06461 |
203-877-0300 |
| Child and Family Guidance Center | OPCC/ CC/MC |
180 Fairfield Avenue Bridgeport, CT 06604 |
203-394-6529 |
| Child Guidance of Mid Fairfield | OPCC/EDT/CC/ MATCH/TF-CBT |
100 East Avenue Norwalk, CT 06851 |
203-299-1315 |
| Child Guidance of Southern CT | OPCC/CC TF-CBT |
103 West Broad Street Stamford, CT 06902 |
203-324-6127 |
| The Center for Family Justice | OPCC/CC/ TF-CBT |
753 Fairfield Avenue Bridgeport, CT 06604 |
203-334-6154 |
| Family Centers | OPCC/TF-CBT | 60 Palmer’s Hill Road Stamford, CT 06902 |
203-324-3167 |
| Lifebridge | OPCC | 475 Clinton Avenue Bridgeport, CT 06694 |
203-368-4291 |
| Norwalk Community Health Centers | TF-CBT | 120 Connecticut Avenue Norwalk, CT 06854 |
203-851-1000 |
| Southwest Community Health Centers | OPCC/TF-CBT | 1046 Fairfield Avenue Bridgeport, CT 06604 |
203-330-6000 |
| Youth Services Bureau (YSB) |
| Name of Agency | Location | Contact |
| Bridgeport Youth Services Bureau | 45 Lyon Terrace Bridgeport, CT 06608 |
203-576-7110 |
| The Depot Youth Center | 25 Heights Road Darien, CT 06820 |
203-655-0812 |
| Fairfield Youth Services | 75 Mill Plain Road Fairfield, CT 06824 |
203-256-3191 |
| Greenwich Youth Services-United Way | 101 Field Point Road Greenwich, CT 06830 |
203-622-3371 |
| New Canaan Youth Services | 77A Main Street New Canaan, CT 06840 |
860-594-3080 |
| Norwalk Department of Youth Services | 125 East Street Norwalk, CT 06851 |
203-854-7785 |
| Stamford Youth Service Bureau | 888 Washington Blvd, 6th Fl Stamford, CT 06901 |
203-977-5674 |
| Stratford Community Services | 468 Birdseye Street Stratford, CT 06615 |
203-385-4095 |
| Trumbull Counseling Center | 5892 Main Street Trumbull, CT 06611 |
203-261-5110 |
| Weston Youth Services | 24 School Road Weston, CT 06883 |
203-222-2585 |
| Westport Social & Youth Services | 110 Myrtle Ave, Rm 200 Westport, CT 06880 |
203-341-1050 |
| Wilton Youth Services | 180 School Road Wilton, CT 06891 |
203-834-6241 |
| School Based Health Centers (SBHC) |
Eligible students are those that attend the schools in which the SBHC is located
*Note Expanded School Health Sites provide medical or behavioral health services where SBHC provides both
| Name of School | Location | Contact |
| Bassick High School | 1181 Fairfield Avenue Bridgeport, CT 06605 |
203-275-3081 |
| Blackham Elementary School | 425 Thorme Street Bridgeport, CT 06606 |
203-275-4751 |
| Central High School | 1 Lincoln Boulevard Bridgeport, CT 06606 |
203-275-1502 |
| Columbus School | 275 George Street Bridgeport, CT 06604 |
203-275-1918 |
| Dunbar Elementary School | 445 Union Avenue Bridgeport, CT 06607 |
203-275-3631 |
| Harding High School | 379 Bond Street Bridgeport, CT 06610 |
203-275-2751 |
| High Horizons Magnet School | 700 Palisade Avenue Bridgeport, CT 06610 |
203-305-7971 |
| Luis Munoz Marin Elementary School | 479 Helen Street Bridgeport, CT 06610 |
203-275-4404 |
| Read Elementary School | 130 Ezra Street Bridgeport, CT 06606 |
203-275-4710 |
| Roosevelt Elementary School | 680 Park Avenue Bridgeport, CT 06604 |
203-275-2100 |
| Brien McMahon High School | 300 Highland Avenue Norwalk, CT 06854 |
203-852-9488 |
| Norwalk High School | 23 Calvin Murphy Drive Norwalk, CT 06851 |
203-838-4881 |
| Cloonan Middle School | 11 W North Street Stamford, CT 06902 |
203-977-4544 |
| Dolan Middle School | 51 Toms Road Stamford, CT 06906 |
203-977-4441 |
| Rippowam Middle School | 381 High Ridge Road Stamford, CT 06905 |
203-977-5255 |
| Stamford High School | 55 Strawberry Hill Avenue Stamford, CT 06902 |
203-977-4223 |
| Westhill High School | 125 Roxbury Road Stamford, CT 06902 |
203-977-4477 |
| Wooster Middle School | 150 Lincoln Street Stratford, CT 06614 |
203-385-4275 |
| Family Resource Centers (FRC) |
| Name | Location | Contact |
| Cesar A. Batalla Elementary School | 606 Howard Avenue Bridgeport, CT 06605 |
203-579-8526 |
| Dunbar School | 445 Union Avenue Bridgeport, CT 06607 |
203-275-3648 |
| Roosevelt School | 680 Park Avenue Bridgeport, CT 06604 |
203-275-2102 |
| Fox Run Elementary School | 228 Fillow Street Norwalk, CT 06850 |
203-899-2326 |
| Side By Side Charter School | 10 Chestnut Street Norwalk, CT 06854 |
203-857-0306 |
| Roger International School | 202 Blachley Road Stamford, CT 06902 |
203-323-0681 |
| Stratford Academy | 719 Birdseye Street Stratford, CT 06615 |
203-381-6992 |
| Regional Behavioral Health Action Organization (RBHAO) overseeing Regional Suicide Advisory Board (RSAB) |
Specific RBHAO town information can be found: https://portal.ct.gov/-/media/DMHAS/Prevention/RBHAOContactspdf.pdf
Specific RSAB town information can be found: https://www.preventsuicidect.org/get-involved/regional-advisory-boards/
| Name of Agency | Service Provided | Location | Contact |
| The Hub: Behavioral Health Action Organization For Southwestern CT, A Program of RYASAP RSAB serving the towns of Bridgeport, Darien, Easton, Fairfield, Greenwich, Monroe, New Canaan, Norwalk, Stamford, Stratford, Trumbull, Weston, Westport, Wilton |
RBHAO RSAB |
2470 Fairfield Avenue, 3rd Fl Bridgeport, CT 06605 |
203-450-3328 |
| National Suicide Prevention Lifeline | https://suicidepreventionlifeline.org/ | 1-800-273-8255 | |
| Crisis Text Line | https://www.crisistextline.org/text-us/ | Text CT to 741741 |
| Statewide Programs |
| Name of Agency | Service Provided | Location | Contact |
| FAVOR, Inc. | Family Advocacy Family Peer Support |
185 Silas Deane Highway Wethersfield, CT 06109 |
860-563-3232 |
| Beacon Health Options | CC/Intensive Care Coordination | 500 Enterprise Drive Rocky Hill, CT 06067 |
877-552-8247 |
Disclaimer: This may not be an exhaustive list of the services available in your area. For additional services, you may reach out to your local children’s behavioral health collaborative listed at www.connectingtocarect.org or contact Infoline 2-1-1 Connecticut at www.211ct.org.
South Central Region Resource List
Updated 10.22.21
For Mobile Crisis, dial 2-1-1, press “1” and “1” again to be directly connected
| Community Based Behavioral Health |
LEGEND | Outpatient Psychiatric Clinics for Children (OPCC) | Extended Day Treatment (EDT) | Care Coordination (CC) | Mobile Crisis (MC) |Modular Approach to Therapy for Children (MATCH) |
Trauma-Focused Cognitive Behavioral Therapy (TF-CBT)
For mobile crisis, dial 2-1-1, press “1” and “1” again to be directly connected
| Name of Agency | Service Provided | Location | Contact |
| Bridges Healthcare, Inc. | OPCC/CC MATCH/TF-CBT |
949 Bridgeport Avenue Milford, CT 06460 |
203-878-6365 |
| Bridges Healthcare, Inc. | OPCC/CC MATCH/TF-CBT |
98 Elm Street West Haven, CT 06516 |
203-878-6365 |
| Children’s Center of Hamden | EDT | 1400 Whitney Avenue Hamden, CT 06517 |
203-248-2116 |
| Clifford Beers Guidance Clinic | OPCC/CC/MC MATCH/TF-CBT |
93 Edwards Street New Haven, CT 06511 |
203-772-1270 |
| Clifford Beers Guidance Clinic | OPCC | 1575 Boston Post Road Building B, Unit C Guilford, CT 06437 |
203-772-1270 |
| Cornell Scott Hill Health Corporation | OPCC TF-CBT | 400 Columbus Avenue New Haven, CT 06519 |
203-503-3055 |
| Lower Naugatuck Valley Parent Child Resource Center, Inc. | OPCC MATCH/TF-CBT | 30 Elizabeth Street Derby, CT 06418 |
203-800-7177 |
| Yale Child Study Center | OPCC MATCH/TF-CBT | 350 George Street, 2nd Fl New Haven, CT 06511 |
844-362-9272 |
| West Haven Mental Health Clinic | OPCC TF-CBT | 270 Center Street West Haven, CT 06516 |
203-974-5900 |
| Youth Services Bureau (YSB) |
| Name of Agency | Location | Contact |
| Ansonia Youth Service Bureau | 42 Grove Street Ansonia, CT 06401 |
203-736-5095 |
| Branford Counseling Center | 342 Harbor Street Branford, CT 06405 |
203-481-4248 |
| Derby Bureau of Youth Services | 1 Elizabeth Street Derby, CT 06418 |
203-736-1450 |
| Town of East Haven Youth Services Bureau | 1 Maple Street East Haven, CT 06512 |
203-415-9394 |
| Guilford Youth and Family Services | 36 Graves Avenue Guilford, CT 06437 |
203-453-8047 |
| Hamden Youth Services Bureau | 11 Pine Street Hamden, CT 06514 |
203-777-2610 |
| Milford Youth and Family Services | 150 Gulf Street Milford, CT 06460 |
203-783-3253 |
| City of New Haven Youth Services Department | 165 Church Street New Haven, CT 06510 |
203-946-7582 |
| North Haven Youth Services | 18 Church Street North Haven, CT 06473 |
203-239-5321 |
| Orange Youth Services | 525 Orange Center Road Orange, CT 06577 |
203-891-4785 |
| Shelton Youth Service Bureau | 120 Meadow Street Shelton, CT 06484 |
203-924-7614 |
| West Haven Youth and Family Services | 201 Noble Street West Haven, CT 06516 |
203-937-3633 |
| Woodbridge Youth Service Bureau | 4 Meetinghouse Lane Woodbridge, CT 06525 |
203-389-3429 |
| School Based Health Centers (SBHC) |
Eligible students are those that attend the schools in which the SBHC is located
*Note Expanded School Health Sites provide medical or behavioral health services where SBHC provides both
| Name of School | Location | Contact |
| Ansonia High School | 20 Pulaski Highway Ansonia, CT 06401 |
203-732-7230 |
| Branford High School | 185 East Main Street Branford, CT 06405 |
203-315-6727 |
| Francis Walsh Intermediate School | 185 Damascus Road Branford, CT 06405 |
203-315-3533 |
| Mary Murphy Elementary School | 14 Brushy Plain Road Branford, CT 06405 |
203-488-4151 |
| Momauguin Elementary School | 99 Cosey Beach Road East Haven, CT 06512 |
203-468-3321 |
| Church Street Elementary | 95 Church Street Hamden, CT 06514 |
203-407-4368 |
| Hamden High School | 2040 Dixwell Avenue Hamden, CT 06514 |
203-248-6107 |
| Augusta Lewis Troup School | 259 Edgewood Avenue New Haven, CT 06511 |
475-220-3076 |
| Barnard Environmental Studies Interdistrict Magnet | 170 Derby Avenue New Haven, CT 06511 |
475-220-3584 |
| Clinton Avenue School | 293 Clinton Avenue New Haven, CT 06513 |
475-220-3318 |
| Fair Haven School | 164 Grand Avenue New Haven, CT 06513 |
475-220-2643 |
| James Hillhouse High School | 480 Sherman Parkway New Haven, CT 06511 |
475-220-7555 |
| King/Robinson Interdistrict Magnet | 150 Fournier Street New Haven, CT 06511 |
475-220-2791 |
| Lincoln-Bassett Community School | 130 Bassett Street New Haven, CT 06511 |
475-220-8516 |
| Mauro-Sheridan Interdistrict Magnet | 191 Fountain Street New Haven, CT 06515 |
475-220-2815 |
| Robert Clemente Leadership Academy | 360 Columbus Avenue New Haven, CT 06519 |
475-220-7617 |
| Truman School | 114 Truman Street New Haven, CT 06519 |
475-220-2122 |
| Wilbur Cross High School | 181 Mitchell Drive New Haven CT 06511 |
475-220-7444 |
| Family Resource Centers (FRC) |
| Name | Location | Contact |
| Indian Neck School | 12 Melrose Avenue Branford, CT 06405 |
203-481-5066 |
| Overbrook Early Learning Center | 54 Gerrish Avenue East Haven, CT 06512 |
203-468-3305 |
| Church Street Elementary | 95 Church Street Hamden, CT 06514 |
203-407-3111 |
| Calf Pen Meadow Middle School | 395 Welchs Point Road Milford, CT 06460 |
203-783-3626 |
| Pumpkin Delight Elementary School | 24 Art Street Milford, CT 06460 |
203-783-3626 |
| Augusta Lewis Troup School | 259 Edgewood Avenue New Haven, CT 06511 |
475-220-3000 |
| Brennan Rogers School of Communications and Media | 200 Wilmot Road New Haven, CT 06515 |
475-220-2221 |
| Fair Haven School | 164 Grand Avenue New Haven, CT 06513 |
475-220-2630 |
| Hill Central School | 144 DeWitt Street New Haven, CT 06519 |
475-220-6195 |
| North Branford Parks and Recreation | 1332 Middletown Avenue Northford, CT 06472 |
203-484-4243 |
| Savin Rock Community School | 50 Park Street West Haven, CT 06516 |
203-931-4739 |
| Regional Behavioral Health Action Organization (RBHAO) overseeing Regional Suicide Advisory Board (RSAB) |
Specific RBHAO town information can be found: https://portal.ct.gov/-/media/DMHAS/Prevention/RBHAOContactspdf.pdf
Specific RSAB town information can be found: https://www.preventsuicidect.org/get-involved/regional-advisory-boards/
| Name | Service Provided | Location | Contact |
| Alliance for Prevention and Wellness/A Program of BHcare RSAB serving the towns of Ansonia, Bethany, Branford, Chester, Clinton, Cromwell, Deep River, Derby, Durham, East Haddam, East Hampton, East Haven, Essex, Guilford, Haddam, Hamden, Killingworth, Lyme, Madison, Meriden, Middlefield, Middletown, Milford, New Haven, North Branford, North Haven, Old Lyme, Old Saybrook, Orange, Portland, Seymour, Shelton, Wallingford, Westbrook, West Haven, Woodbridge |
RBHAO RSAB |
127 Washington Ave, 3rd Fl North Haven, CT 06473 |
203-736-8566 |
| National Suicide Prevention Lifeline | https://suicidepreventionlifeline.org/ | 1-800-273-8255 | |
| Crisis Text Line | https://www.crisistextline.org/text-us/ | Text CT to 741741 |
| Statewide Programs |
| Name of Agency | Service Provided | Location | Contact |
| FAVOR, Inc. | Family Advocacy Family Peer Support |
185 Silas Deane Highway Wethersfield, CT 06109 |
860-563-3232 |
| Beacon Health Options | CC/Intensive Care Coordination | 500 Enterprise Drive Rocky Hill, CT 06067 |
877-552-8247 |
Disclaimer: This may not be an exhaustive list of the services available in your area. For additional services, you may reach out to your local children’s behavioral health collaborative listed at www.connectingtocarect.org or contact Infoline 2-1-1 Connecticut at www.211ct.org.
Eastern Region Resource List
Updated 10.22.21
For Mobile Crisis, dial 2-1-1, press “1” and “1” again to be directly connected
| Community Based Behavioral Health |
LEGEND | Outpatient Psychiatric Clinics for Children (OPCC) | Extended Day Treatment (EDT) | Care Coordination (CC) | Mobile Crisis (MC) |Modular Approach to Therapy for Children (MATCH) |
Trauma-Focused Cognitive Behavioral Therapy (TF-CBT)
For mobile crisis, dial 2-1-1, press “1” and “1” again to be directly connected
| Name of Agency | Service Provided | Location | Contact |
| Child and Family Agency of SE CT | OPCC/MATCH/TF-CBT | 7 Vauxhall Street New London, CT 06320 |
860-443-2896 |
| Child and Family Agency of SE CT | OPCC/MATCH/TF-CBT | 190 Westbrook Road Essex, CT 06426 |
860-767-0147 |
| Clifford Beers Guidance Clinic | MC | 93 Edwards Street New Haven, CT 06511 |
203-772-1270 |
| Community Health Center | OPCC/TF-CBT | 675 Main Street Middletown, CT 06457 |
860-347-6971 |
| Community Health Resources | OPCC/MATCH/TF-CBT | 1310 West Main Street Willimantic, CT 06226 |
860-456-7200 |
| Community Health Resources | CC | 1491 West Main Street Willimantic, CT 06226 |
877-884-3571 or 860-771-4865 |
| Middlesex Hospital | MC | 51 Broad Street Middletown, CT 06457 |
860-358-3401 |
| Natchaug Hospital | EDT | 189 Storrs Road Mansfield Center, CT 06250 |
860-465-5943 |
| Natchaug Hospital | EDT | 934 North Main Street Danielson, CT 06239 |
860-779-2101 x315 |
| Natchaug Hospital | EDT | 1353 Gold Star Highway Groton, CT 06340 |
860-465-5907 |
| Natchaug Hospital | EDT | 11-A Stott Avenue Norwich, CT 06360 |
860-823-5320 |
| Rushford Center Inc. | CC | 883 Paddock Avenue Meriden, CT 06450 |
860-349-2043 |
| United Community & Family Services | MC | 31 Dow Road Plainfield, CT 06374 |
860-822-4317 |
| United Community & Family Services | MC | 77 East Town Street Norwich, CT 06360 |
860-822-4317 |
| United Community & Family Services | OPCC/CC/ MATCH/TF-CBT |
47 Town Street Norwich, CT 06360 |
860-892-7042 |
| United Services, Inc. | OPCC MATCH/TF-CBT |
140 North Frontage Road Mansfield Center, CT 06250 |
860-456-2261 |
| United Services, Inc. | OPCC MATCH/TF-CBT |
1007 North Main Street Dayville, CT 06241 |
860-774-2020 |
| Village for Families & Children | EDT | 282 Main Street Ext Middletown, CT 06457 |
860-236-4511 x3636 |
| Wheeler Clinic | EDT | 20 Tuttle Place, Unit 6A Middletown, CT 06457 |
860-632-3231 |
| Youth Services Bureau (YSB) |
| Name of Agency | Location | Contact |
| Ashford Youth Services Bureau | 5 Town Hall Road Ashford, CT 06278 |
860-487-4417 |
| Clinton Youth & Family Services | 48 East Main Street Clinton, CT 06413 |
860-669-1103 |
| Colchester Youth Services | 127 Norwich Ave, Ste 205 Colchester, CT 06415 |
860-537-7255 |
| Coventry Youth Services | 1712 Main Street Coventry, CT 06238 |
860-742-5324 |
| Cromwell Youth Services | 41 West Street Cromwell, CT 06416 |
860-632-3448 |
| Durham/Middlefield Youth & Family Services | 405 Main Street, Ste 11 Middlefield, CT 06455 |
860-349-0258 |
| East Haddam Youth & Family Services | 387 East Haddam-Moodus Road Moodus, CT 06469 |
860-873-3296 |
| East Hampton Youth Services | 20 East High Street East Hampton, CT 06424 |
860-267-9982 |
| East Lyme Youth Services (includes Salem) | 45 Society Road Niantic, CT 06357 |
860-739-6788 |
| Griswold Community Youth Center | 28 Main Street Jewett City, CT 06351 |
860-376-7026 |
| Groton Youth Service Bureau | 45 Fort Hill Road Groton, CT 06340 |
860-441-6760 |
| Youth and Family Services of Haddam - Killingworth, Inc. | 91 Little City Road Higganum, CT 06441 |
860-345-7498 |
| Ledyard Youth Services (Ledyard, Gales Ferry) | 741 Colonel Ledyard Hwy Ledyard, CT 06339 |
860-464-3213 |
| Lyme’s Youth Service Bureau (Lyme, Old Lyme) | 59 Lyme Street Old Lyme, CT 06371 |
860-434-7208 |
| Madison Youth Services | 10 School Street Madison, CT 06443 |
203-245-5645 |
| Mansfield Youth Services | 4 South Eagleville Road Mansfield, CT 06268 |
860-429-3319 |
| Middletown Youth Services | 51 Green Street Middletown, CT 06457 |
860-854-6030 |
| Montville Youth Services | 836 Old Colchester Road Oakdale, CT 06370 |
860-848-7724 |
| New London Office of Youth Affairs | 111 Union Street New London, CT 06320 |
860-442-4994 |
| Norwich Youth & Family Services | 75 Mohegan Road Norwich, CT 06360 |
860-823-3782 |
| Old Saybrook Youth and Family | 322 Main Street Old Saybrook, CT 06475 |
860-395-3190 |
| Portland Youth Service Bureau | 265 Main Street Portland, CT 06480 |
860-342-6758 |
| Preston Youth Service Bureau | 389 Route 2 Preston, CT 06365 |
860-887-5581 |
| Stonington Youth Services | 166 South Broad Street Pawcatuck, CT 06379 |
860-535-5015 |
| TEEG | 15 Thatcher Road N. Grosvenordale, CT 06255 |
860-923-3458 |
| Tri-Town Youth Services (Chester, Deep River, Essex) |
56 High Street Deep River, CT 06417 |
860-526-3600 |
| United Services, Inc (Brooklyn, Canterbury, Eastford, Killingly, Plainfield, Sterling) |
P.O. Box 378 Wauregan, CT 06387 |
860-564-6100 |
| Voluntown Youth Services | 195 Main Street Voluntown, CT 06384 |
860-376-2325 |
| Waterford Youth Service Bureau | 200 Boston Post Road Waterford, CT 06385 |
860-444-5848 |
| Westbrook Youth and Family Services | 1163 Boston Post Road Westbrook, CT 06498 |
860-399-9239 |
| Willington Youth Services | 40 Old Farms Road Willington, CT 06279 |
860-429-8321 |
| Windham Youth Services (Willimantic, Windham) | 872 Main Street Willimantic, CT 06226 |
860-423-4534 |
| School Based Health Centers (SBHC) |
Eligible students are those that attend the schools in which the SBHC is located
*Note Expanded School Health Sites provide medical or behavioral health services where SBHC provides both
| Name of School | Location | Contact |
| Parish Hill High/Middle School* | 304 Parish Hill Road Chaplin, CT 06235 |
860-455-9584 |
| Catherine Kolnaski Magnet School | 500 Poquonnock Road Groton, CT 06340 |
860-445-2191 |
| Fitch High School | 101 Groton Long Point Road Groton, CT 06340 |
860-446-9543 or 860-449-7253 |
| Groton Middle School | 35 Groton Long Point Road Groton, CT 06340 |
860-446-4200 |
| Thames River Magnet School | 250 Brandegee Avenue Groton, CT 06340 |
860-980-8230 temporary |
| Jeffrey Elementary School* | 331 Copse Road Madison, CT 06443 |
203-245-6340 |
| Ryerson Elementary School* | 982 Durham Road Madison, CT 06443 |
203-245-6340 |
| Beman Middle School | 1 Wilderman’s Way Middletown, CT 06457 |
860-347-8594 |
| Commodore Macdonough Elementary School | 66 Spring Street Middletown, CT 06457 |
860-347-8553 |
| Wesley Elementary | 10 Wesleyan Hills Road Middletown, CT 06457 |
860-344-0381 |
| Mystic River Magnet School | 160 Fishtown Road Mystic, CT 06355 |
860-908-8300 |
| Stonington Middle School | 204 Mistuxet Ave Mystic, CT 06355 |
860-536-9613 x4112 |
| Bennie Dover Jackson Middle School | 36 Waller Street New London, CT 06320 |
860-437-6480 x7232 |
| ISAAC (Interdistrict School for Arts and Communications) | 190 Governor Winthrop Blvd New London, CT 06320 |
860-447-1003 |
| Jennings Elementary School | 50 Mercer Street New London, CT 06320 |
860-447-6050 x7665 |
| Nathan Hale Elementary School | 37 Beech Drive New London, CT 06320 |
860-447-6060 x7537 |
| New London High School | 490 Jefferson Avenue New London, CT 06320 |
860-437-6400 x7019 |
| Regional Multicultural Magnet School | 1 Bulkeley Place New London, CT 06320 |
860-437-7775 x7333 |
| Winthrop Elementary School | 74 Grove Street New London, CT 06320 |
860-447-6070 x7115 |
| Barrows STEM Academy | 141 Tuckie Road North Windham, CT 06226 |
860-465-2610, x4610 |
| Putnam Middle School* | 35 Wicker Street Putnam, CT 06260 |
860-928-4698 Elem/middle or 860-928-2714 High school |
| Friendship School | 24 Rope Ferry Road Waterford, CT 06385 |
860-447-4049 x7156 |
| Windham High School | 355 High Street Willimantic, CT 06226 |
860-465-2465 |
| Windham Middle School | 123 Quarry Street Willimantic, CT 06226 |
860-465-2620 |
| Family Resource Centers (FRC) |
| Name | Location | Contact |
| Catherine C. Kolnaski Magnet School | 500 Poquonnock Road Groton, CT 06340 |
860-448-5586 |
| Farm Hill School | 390 Ridge Road Middletown, CT 06457 |
860-347-0869 |
| Jennings School | 50 Mercer Street New London, CT 06320 |
860-448-5294 |
| Nathan Hale School | 37 Beech Drive New London, CT |
860-448-5049 |
| Thomas W. Mahan Elementary School | 94 Salem Turnpike Norwich, CT 06360 |
860-823-4205 |
| Plainfield’s Early Childhood Center | 651 Norwich Road Plainfield, CT 06374 |
860-564-6411 |
| Putnam Elementary School | 33 Wicker Street Putnam, CT 06260 |
860-963-6940 |
| Goodyear E.C.C. | 22 Williamsville Road Rogers, CT 06263 |
860-779-6770 |
| Natchaug Elementary School | 123 Jackson Street Willimantic, CT 06226 |
860-465-2396 or 860-465-2578 |
| Regional Behavioral Health Action Organization (RBHAO) overseeing Regional Suicide Advisory Board (RSAB) |
Specific RBHAO town information can be found: https://portal.ct.gov/-/media/DMHAS/Prevention/RBHAOContactspdf.pdf
Specific RSAB town information can be found: https://www.preventsuicidect.org/get-involved/regional-advisory-boards/
| Name | Service Provided | Location | Contact |
| Alliance for Prevention and Wellness/A Program of BHcare | RBHAO RSAB |
127 Washington Ave, 3rd Fl North Haven, CT 06473 |
203-736-8566 |
| Alliance for Prevention and Wellness serving the towns of Ansonia, Bethany, Branford, Chester, Clinton, Cromwell, Deep River, Derby, Durham, East Haddam, East Hampton, East Haven, Essex, Guilford, Haddam, Hamden, Killingworth, Lyme, Madison, Meriden, Middlefield, Middletown, Milford, New Haven, North Branford, North Haven, Old Lyme, Old Saybrook, Orange, Portland, Seymour, Shelton, Wallingford, Westbrook, West Haven, Woodbridge | |||
| SERAC | RBHAO RSAB |
228 West Town Street Norwich, CT 06360 |
860-848-2800 |
| SERAC serving the towns of Ashford, Bozrah, Brooklyn, Canterbury, Chaplin, Colchester, Columbia, Coventry, East Lyme, Eastford, Franklin, Griswold, Groton, Hampton, Killingly, Lebanon, Ledyard, Lisbon, Lyme, Mansfield, Montville, New London, North Stonington, Norwich, Old Lyme, Plainfield, Pomfret, Preston, Putnam, Salem, Scotland, Sprague, Sterling, Stonington, Thompson, Union, Voluntown, Waterford, Willington, Windham, Woodstock | |||
| National Suicide Prevention Lifeline | https://suicidepreventionlifeline.org/ | 1-800-273-8255 | |
| Crisis Text Line | https://www.crisistextline.org/text-us/ | Text CT to 741741 | |
| Statewide Programs |
| Name of Agency | Service Provided | Location | Contact |
| FAVOR, Inc. | Family Advocacy Family Peer Support |
185 Silas Deane Highway Wethersfield, CT 06109 |
860-563-3232 |
| Beacon Health Options | CC/Intensive Care Coordination | 500 Enterprise Drive Rocky Hill, CT 06067 |
877-552-8247 |
Disclaimer: This may not be an exhaustive list of the services available in your area. For additional services, you may reach out to your local children’s behavioral health collaborative listed at www.connectingtocarect.org or contact Infoline 2-1-1 Connecticut at www.211ct.org.
North Central Region Resource List
Updated 10.22.21
For Mobile Crisis, dial 2-1-1, press “1” and “1” again to be directly connected
| Community Based Behavioral Health |
LEGEND | Outpatient Psychiatric Clinics for Children (OPCC) | Extended Day Treatment (EDT) | Care Coordination (CC) | Mobile Crisis (MC) |Modular Approach to Therapy for Children (MATCH) |
Trauma-Focused Cognitive Behavioral Therapy (TF-CBT)
For mobile crisis, dial 2-1-1, press “1” and “1” again to be directly connected
| Name of Agency | Service Provided | Location | Contact |
| Bridge Family Center | OPCC | 26 Union Street, Ste 2 Rockville, CT 06066 |
860-313-1119 |
| Bridge Family Center | OPCC | 100 Shield Street West Hartford, CT 06110 |
860-313-1119 |
| Catholic Charities | OPCC/TF-CBT | 45 Wadsworth Street Hartford, CT 06106 |
860-527-1124 |
| Community Child Guidance Clinic | OPCC/ MATCH/TF-CBT |
317 North Main Street Manchester, CT 06042 |
860-643-2101 |
| Community Health Resources | MC/CC/MATCH/TF-CBT | 444 Center Street Manchester, CT 06040 |
860-730-8956 |
| Community Health Resources | OPCC/MATCH/TF-CBT | 153 Hazard Avenue Enfield, CT 06082 |
860-253-5020 |
| Community Health Resources | OPCC/CC/TF-CBT/MATCH | 693 Bloomfield Ave, Ste 101 Bloomfield, CT 06002 |
860-243-6584 |
| Hartford Hospital (Institute of Living) | OPCC/EDT | 200 Retreat Avenue Hartford, CT 06106 |
860-545-7200 |
| Hockanum Valley Community Council | OPCC | 27 Naek Road, Ste 4 Vernon, CT 06066 |
860-872-9825 |
| Klingberg Family Center | OPCC | 157 Charter Oak Avenue Hartford, CT 06106 |
860-243-4416 |
| Village for Families & Children | OPCC/EDT MATCH/TF-CBT |
331 Wethersfield Avenue Hartford, CT 06114 |
860-236-4511 |
| Village for Families & Children | EDT | 34 Sequassen Street Hartford, CT 06106 |
860-263-4511 |
| Village for Families & Children | EDT | 317 North Main Street Manchester, CT 06040 |
860-236-4511 |
| Wheeler Clinic | CC | 43 Woodland Street Hartford, CT 06105 |
860-793-3551 |
| Wheeler Clinic | OPCC/MC/ MATCH/TF-CBT |
43 Woodland Street Hartford, CT 06105 |
860-793-3500 |
| Youth Services Bureau (YSB) |
| Name of Agency | Location | Contact |
| AHM (Andover, Hebron, Marlborough) Youth Services | 25 Pendleton Drive Hebron, CT 06248 |
860-228-9488 |
| Bloomfield Youth Services | 330 Park Ave, 2nd Fl Bloomfield, CT 06002 |
860-242-1895 |
| East Granby Youth Services | 9 Center Street East Granby, CT 06026 |
860-653-7800 |
| East Hartford Youth Services | 50 Chapman Place East Hartford, CT 06108 |
860-291-7179 |
| Ellington Youth Services | 31 Arbor Lane Ellington, CT 06029 |
860-870-3130 |
| Enfield Youth Services | 19 North Main Street Enfield, CT 06082 |
860-253-6380 |
| Glastonbury Youth Services | 321 Hubbard Street Glastonbury, CT 06033 |
860-652-7673 |
| Granby Youth Services | 15C North Granby Road Granby, CT 06035 |
860-844-5355 |
| Hartford Dept. of Families, Children, Youth & Recreation | 550 Main Street, Room 305 Hartford, CT 06103 |
860-757-9595 |
| Manchester Youth Services | 63 Linden Street Manchester, CT 06040 |
860-647-5213 |
| Somers Social Services | 619 Main Street Somers, CT 06071 |
860-265-7551 |
| South Windsor Youth Services | 150 Nevers Road South Windsor, CT 06074 |
860-648-5050 |
| Stafford Family Services | 21 Hyde Park Road Stafford Springs, CT 06076 |
860-684-4239 |
| Suffield Youth Services | 145 Bridge Street Suffield, CT 06078 |
860-668-3329 x3329 |
| Tolland Youth Services | 21 Tolland Green Tolland, CT 06084 |
860-871-3612 |
| Vernon Youth Services | 9 Elm Street Vernon, CT 06066 |
860-870-3555 |
| The Bridge Family Center (West Hartford) | 1038 Farmington Avenue West Hartford, CT 06107 |
860-313-1119 |
| Windsor Youth Services | 599 Matianuck Avenue Windsor, CT 06095 |
860-285-1946 |
| Windsor Locks Youth Services | 50 Church Street Windsor Locks, CT 06096 |
860-627-1482 |
| School Based Health Centers (SBHC) |
Eligible students are those that attend the schools in which the SBHC is located
*Note Expanded School Health Sites provide medical or behavioral health services where SBHC provides both
| Name of School | Location | Contact |
| CREC Metropolitan Learning Center | 1551 Blue Hills Avenue Bloomfield, CT 06002 |
860-242-7834 |
| Dr. John A. Langford Elementary School | 61 Alps Drive East Hartford, CT 06108 |
860-622-5714 |
| Early Childhood Learning Center at Hockanum | 191 Main Street East Hartford, CT 06118 |
860-622-5450 |
| East Hartford High School | 869 Forbes Street East Hartford, CT 06118 |
860-622-5340 |
| East Hartford Middle School | 777 Burnside Avenue East Hartford, CT 06108 |
860-622-5670 |
| Franklin H. Mayberry Elementary School | 101 Great Hill Road East Hartford, CT 06108 |
860-622-5731 |
| Silver Lane Elementary School | 15 Mercer Avenue East Hartford, CT 06118 |
860-622-1250 x1 |
| Synergy Alternative High School | 40 Butternut Drive East Hartford, CT 06118 |
860-622-5984 |
| East Windsor High School | 76 South Main Street East Windsor, CT 06088 |
860-623-3361 x7247 |
| Buckley High School | Grades 9-10: 585 Wethersfield Avenue Hartford, CT 06114 Grades 11-12: 395 Lyme Street Hartford, CT 06112 |
860-695-1014 |
| Dwight Bellizzi Dual Language Academy | 215 South Street Hartford, CT 06114 |
860-695-2444 |
| Hartford Public High School | 55 Forest Street Hartford, CT 06105 |
860-695-1359 |
| Maria C. Colon Sanchez School | 176 Babcock Street Hartford, CT 06106 |
860-695-4943 |
| Martin Luther King Jr. School | 25 Ridgefield Street Hartford, CT 06112 |
860-695-0303 |
| M.D. Fox Elementary School | 470 Maple Avenue Hartford, CT 06114 |
860-695-7732 |
| Sarah J. Rawson Elementary School | 260 Holcomb Street Hartford, CT 06112 |
860-695-4842 |
| Weaver High School | 415 Granby Street Hartford, CT 06112 |
860-695-1682 |
| Family Resource Centers (FRC) |
| Name | Location | Contact |
| Laurel School | 1 Filley Street Bloomfield, CT 06002 |
860-769-5518 |
| Franklin H Mayberry School | 101 Great Hill Road East Hartford, CT 06108 |
860-622-5737 |
| Silver Lane School | 15 Mercer Avenue East Hartford, CT 06108 |
860-622-5515 |
| Broad Brook School | 14 Rye Street East Windsor, CT 06016 |
860-627-9741 |
| Henry Barnard School | 27 Shaker Road Enfield, CT 06082 |
860-253-5144 |
| Stowe Family Resource Center | 117 Post Office Road Enfield, CT 06082 |
860-253-5214 |
| Burns Latino Studies Academy | 195 Putnam Street Hartford, CT 06106 |
860-695-2994 |
| Fred D. Wish Museum School | 350 Barbour Street Hartford, CT 06120 |
860-695-5639 |
| Maria C. Colon Sanchez School | 176 Babcock Street Hartford, CT 06106 |
860-695-4940 |
| Sarah J. Rawson Elementary School | 260 Holcomb Street Hartford, CT 06112 |
860-695-6867 |
| S.A.N.D School | 1750 Main Street Hartford, CT 06120 |
860-695-5062 |
| Gilead Hill School | 580 Gilead Street Hebron, CT 06248 |
860-228-9488 |
| Washington Media Arts Magnet School | 94 Cedar Street Manchester, CT 06040 |
860-647-3330 |
| Birch Grove Primary School | 247 Rhodes Road Tolland, CT 06084 |
860-870-6750 x30216 |
| Maple Street School | 20 Maple Street Vernon, CT 06066 |
860-335-6954 |
| Charter Oak International Academy | 425 Oakwood Avenue West Hartford, CT 06110 |
860-929-5575 |
| Oliver Ellsworth School | 730 Kennedy Road Windsor, CT 06095 |
860-687-2070 |
| Regional Behavioral Health Action Organization (RBHAO) overseeing Regional Suicide Advisory Board (RSAB) |
Specific RBHAO town information can be found: https://portal.ct.gov/-/media/DMHAS/Prevention/RBHAOContactspdf.pdf
Specific RSAB town information can be found: https://www.preventsuicidect.org/get-involved/regional-advisory-boards/
| Name | Service Provided | Location | Contact |
| Amplify, Inc. | RBHAO RSAB |
151 New Park Ave, Ste 14A Hartford, CT 06106 |
860-667-6388 |
| Serving towns of Andover, Avon, Berlin, Bloomfield, Bolton, Bristol, Burlington, Canton, East Granby, East Hartford, East Windsor, Ellington, Enfield, Farmington, Glastonbury, Granby, Hartford, Hebron, Kensington, Manchester, Marlborough, New Britain, Newington, Plainville, Plymouth, Rocky Hill, Simsbury, Somers, South Windsor, Southington, Stafford, Suffield, Tolland, Vernon, West Hartford, Wethersfield, Windsor, Windsor Locks | |||
| National Suicide Prevention Lifeline | https://suicidepreventionlifeline.org/ | 1-800-273-8255 | |
| Crisis Text Line | https://www.crisistextline.org/text-us/ | Text CT to 741741 | |
| Statewide Programs |
| Name of Agency | Service Provided | Location | Contact |
| FAVOR, Inc. | Family Advocacy Family Peer Support |
185 Silas Deane Highway Wethersfield, CT 06109 |
860-563-3232 |
| Beacon Health Options | CC/Intensive Care Coordination | 500 Enterprise Drive Rocky Hill, CT 06067 |
877-552-8247 |
Disclaimer: This may not be an exhaustive list of the services available in your area. For additional services, you may reach out to your local children’s behavioral health collaborative listed at www.connectingtocarect.org or contact Infoline 2-1-1 Connecticut at www.211ct.org.
Western Region Resource List
Updated 10.22.21
For Mobile Crisis, dial 2-1-1, press “1” and “1” again to be directly connected
| Community Based Behavioral Health |
LEGEND | Outpatient Psychiatric Clinics for Children (OPCC) | Extended Day Treatment (EDT) | Care Coordination (CC) | Mobile Crisis (MC) |Modular Approach to Therapy for Children (MATCH) |
Trauma-Focused Cognitive Behavioral Therapy (TF-CBT)
For mobile crisis, dial 2-1-1, press “1” and “1” again to be directly connected
| Name of Agency | Service Provided | Location | Contact |
| Charlotte Hungerford | OPCC/EDT MATCH/TF-CBT |
50 Litchfield Street Torrington, CT 06790 |
860-489-3391 |
| Community Mental Health Affiliates | OPCC/EDT MATCH/TF-CBT |
255 Bank Street, 4th Fl Waterbury, CT 06704 |
860-596-9724 |
| Family and Children’s Aid, Inc. | OPCC/EDT TF-CBT |
75 West Street Danbury, CT 06810 |
203-205-2616 |
| Family and Children’s Aid, Inc. | OPCC | 325 Danbury Road New Milford, CT 06776 |
860-354-8556 |
| Family and Children’s Aid, Inc. | OPCC/EDT TF-CBT |
30 Holmes Avenue Waterbury, CT 06702 |
203-755-2868 |
| Wellmore, Inc. | OPCC/CC MATCH/TF-CBT |
141 East Main Street, 2nd Fl Waterbury, CT 06702 |
203-756-7287 |
| Wellmore, Inc. | OPCC | 333 Church Street, 1st Fl Naugatuck, CT 06770 |
203-723-9599 |
| Wellmore, Inc. | MC/CC | 402 E. Main Street Waterbury, CT 06702 |
203-755-1143 |
| Wellmore, Inc. | MC/CC | 30 Peck Road, Bldg 2 Ste 2203 Torrington, CT 06790 |
860-626-7007 |
| Youth Services Bureau (YSB) |
| Name of Agency | Location | Contact |
| Danbury Youth Services, Inc. | 91 West Street Danbury, CT 06810 |
203-748-2936 |
| Housatonic Youth Service Bureau, Inc. | 246 Warren Turnpike Falls Village, CT 06031 |
860-824-4720 |
| Naugatuck Youth Services | 13 Scott Street Naugatuck, CT 06770 |
203-720-5673 |
| New Milford Youth Agency | 2 Pickett District Road New Milford, CT 06776 |
860-210-2030 |
| Newtown Youth and Family Services | 15 Berkshire Road Sandy Hook, CT 06482 |
203-270-4335 |
| Torrington Youth Service Bureau | 8 Church Street Torrington, CT 06790 |
860-496-0356 |
| Ridgefield Youth Service Bureau | 90 East Road Ridgefield, CT 06877 |
203-438-6141 |
| Waterbury Youth Services | 83 Prospect Street Waterbury, CT 06702 |
203-573-0264 |
| WatertownYouth Services | 250 Colonial Street Oakville, CT 06795 |
860-945-4830 x2100 |
| Winchester Youth Services | 480 Main Street Winchester, CT 06098 |
860-379-0708 x211 |
| School Based Health Centers (SBHC) |
Eligible students are those that attend the schools in which the SBHC is located
*Note Expanded School Health Sites provide medical or behavioral health services where SBHC provides both
| Name of School | Location | Contact |
| Broadview Middle School | 72 Hospital Avenue Danbury, CT 06810 |
203-731-8274 |
| Danbury High School | 43 Clapboard Ridge Road Danbury CT 06811 |
203-790-2886 |
| Rogers Park Middle School | 21 Memorial Drive Danbury, CT 06810 |
203-778-7479 |
| Newtown Middle School | 11 Queen Street Newtown, CT 06470 |
203-270-6114 |
| Crosby High School | 3465 East Main Street Waterbury, CT 06705 |
203-805-4916 |
| Driggs Elementary School | 77 Woodlawn Terrace Waterbury, CT 06710 |
203-596-9503 |
| Wallace Middle School | 3465 East Main Street Waterbury, CT 06705 |
203-805-4916 |
| Family Resource Centers (FRC) |
| Name | Location | Contact |
| Morris Street School | 28 Morris Street Danbury, CT 06810 |
203-790-2682 |
| Vogel-Wetmore School | 68 Church Street Torrington, CT 06790 |
860-489-8552 |
| Reed School | 33 Griggs Street Waterbury, CT 06704 |
203-574-8180 |
| Woodrow Wilson School | 235 Birch Street Waterbury, CT 06704 |
203-573-6664 |
| Batcheller Early Education Center | 201 Pratt Street Winsted, CT 06098 |
860-379-5423 x5262 |
| Regional Behavioral Health Action Organization (RBHAO) overseeing Regional Suicide Advisory Board (RSAB) |
Specific RBHAO town information can be found: https://portal.ct.gov/-/media/DMHAS/Prevention/RBHAOContactspdf.pdf
Specific RSAB town information can be found: https://www.preventsuicidect.org/get-involved/regional-advisory-boards/
| Name | Service Provided | Location | Contact |
| Western CT Coalition | RBHAO RSAB |
7 Old Sherman Turnpike Danbury, CT 06810 |
203-743-7741 |
| Serving: Barkhamsted, Beacon Falls, Bethel, Bethlehem, Bridgewater, Brookfield, Canaan, Cheshire, Colebrook, Cornwall, Danbury, Goshen, Hartland, Harwinton, Kent, Litchfield, Middlebury, Morris, Naugatuck, New Fairfield, New Hartford, New Milford, Newtown, Norfolk, North Canaan, Oxford, Prospect, Redding, Ridgefield, Roxbury, Salisbury, Sharon, Sherman, Southbury, Thomaston, Torrington, Warren, Washington, Waterbury, Watertown, Winchester, Winsted, Wolcott, and Woodbury | |||
| National Suicide Prevention Lifeline | https://suicidepreventionlifeline.org/ | 1-800-273-8255 | |
| Crisis Text Line | https://www.crisistextline.org/text-us/ | Text CT to 741741 | |
| Statewide Programs |
| Name of Agency | Service Provided | Location | Contact |
| FAVOR, Inc. | Family Advocacy Family Peer Support |
185 Silas Deane Highway Wethersfield, CT 06109 |
860-563-3232 |
| Beacon Health Options | CC/Intensive Care Coordination | 500 Enterprise Drive Rocky Hill, CT 06067 |
877-552-8247 |
Disclaimer: This may not be an exhaustive list of the services available in your area. For additional services, you may reach out to your local children’s behavioral health collaborative listed at www.connectingtocarect.org or contact Infoline 2-1-1 Connecticut at www.211ct.org.
Central Region Resource List
Updated 10.22.21
For Mobile Crisis, dial 2-1-1, press “1” and “1” again to be directly connected
| Community Based Behavioral Health |
LEGEND | Outpatient Psychiatric Clinics for Children (OPCC) | Extended Day Treatment (EDT) | Care Coordination (CC) | Mobile Crisis (MC) |Modular Approach to Therapy for Children (MATCH) |
Trauma-Focused Cognitive Behavioral Therapy (TF-CBT)
For mobile crisis, dial 2-1-1, press “1” and “1” again to be directly connected
| Name of Agency | Service Provided | Location | Contact |
| Bridge Family Center | OPCC | 45 West Main Street Avon, CT 06001 |
860-313-1119 |
| Child Guidance Clinic of Central CT | OPCC MATCH/TF-CBT |
384 Pratt Street Meriden, CT 06450 |
203-235-5767 |
| Community Mental Health Affiliates | OPCC/ MATCH/TF-CBT |
233 Main Street New Britain, CT 06051 |
860-224-8192 |
| Klingberg Family Services | OPCC/EDT | 370 Linwood Avenue New Britain, CT 06052 |
OPCC 860-243-4416 EDT 860-832-5527 |
| Rushford/Hartford HealthCare | CC | 883 Paddock Avenue Meriden, CT 06450 |
860-227-0321 |
| Village for Families & Children | EDT | 117 Lincoln Street Meriden, CT 06451 |
860-236-4511 |
| Wheeler Clinic | OPCC/EDT/CC/MC MATCH/TF-CBT |
91 Northwest Drive Plainville, CT 06062 |
860-793-3500 |
| Wheeler Clinic | OPCC | 225 North Main Street Bristol, CT 06011 |
860-793-3500 |
| Youth Services Bureau (YSB) |
| Name of Agency | Location | Contact |
| Avon Youth Services | 60 West Main Street, Bldg 1 Avon, CT 06001 |
860-409-4394 |
| Berlin Youth Services | 240 Kensington Road Berlin, CT 06037 |
860-828-7059 |
| Bristol Youth Service Bureau | 51 High Street Bristol, CT 06010 |
860-314-4690 |
| Torrington Youth Service Bureau (Torrington, Harwinton, Burlington, Litchfield, Goshen) | 8 Church Street Torrington, CT 06790 |
860-496-0356 |
| Canton Youth Service Bureau | P.O. Box 168 4 Market Street Collinsville, CT 06022 |
860-693-5808 |
| Cheshire Youth Services | 84 South Main Street Cheshire, CT 06410 |
203-271-6690 |
| Farmington Youth Services | 1 Monteith Drive Farmington, CT 06032 |
860-675-2390 |
| Meriden Youth Services | 165 Miller Street Meriden, CT 06450 |
203-630-4239 |
| New Britain Youth and Family Services | 27 West Main Street New Britain, CT 06051 |
860-826-3370 |
| Newington Youth Service Bureau | 200 Garfield Street Newington, CT 06111 |
860-665-8590 |
| Plainville Youth Services | 50 Whiting Street Plainville, CT 06062 |
860-793-0221 |
| Rocky Hill Youth and Family Services | 699 Old Main Street Rocky Hill, CT 06067 |
860-258-2724 |
| Simsbury Youth Services | 754 Hopmeadow Street Simsbury, CT 06070 |
860-658-3283 |
| Southington Youth Services | 196 North Main Street Southington, CT 06489 |
860-276-6281 |
| Wallingford Youth and Social Services | 6 Fairfield Boulevard Wallingford, CT 06492 |
203-294-2175 |
| Wethersfield Social and Youth Services | 505 Silas Deane Highway Wethersfield, CT 06109 |
860-721-2977 |
| School Based Health Centers (SBHC) |
Eligible students are those that attend the schools in which the SBHC is located
*Note Expanded School Health Sites provide medical or behavioral health services where SBHC provides both
| Name of School | Location | Contact |
| Lincoln Middle School | 164 Centennial Avenue Meriden, CT 06451 |
203-238-2381 |
| Benjamin Franklin Elementary School* | 426 West Main Street Meriden, CT 06451 |
203-235-7997 |
| Casimir Pulaski Elementary* | 100 Clearview Avenue Meriden, CT 06450 |
203-238-1273 |
| Hanover Elementary School* | 208 Main Street Meriden, CT 06451 |
203-235-6359 |
| Israel Putnam Elementary School* | 133 Parker Avenue Meriden, CT 06450 |
203-237-8493 |
| John Barry Elementary School* | 124 Columbia Street Meriden, CT 06450 |
203-237-8831 |
| Nathan Hale Elementary School* | 277 Atkins Street Extension Meriden, CT 06450 |
203-237-7486 |
| Roger Sherman Elementary School* | 64 North Pearl Street Meriden, CT 06450 |
203-238-1286 |
| Thomas Hooker Elementary School* | 70 Overlook Road Meriden, CT 06450 |
203-237-8839 |
| Gaffney School | 322 Slater Road New Britain, CT 06053 |
860-438-7822 |
| New Britain High School | 110 Mill Street New Britain, CT 06051 |
860-826-8845 |
| Roosevelt School* | 40 Goodwin Street New Britain, CT 06051 |
860-826-2321 |
| Family Resource Centers (FRC) |
| Name | Location | Contact |
| Greene Hills School | 718 Pine Street Bristol, CT 06010 |
860-584-7822 |
| South Side School | 21 Tuttle Road Bristol, CT 06010 |
860-584-7812 |
| West Bristol School | 500 Clark Avenue Bristol, CT 06010 |
860-584-7815 |
| Benjamin Franklin Elementary School | 426 West Main Street Meriden, CT 06451 |
203-238-2316 |
| John Barry Elementary School | 124 Columbia Street Meriden, CT 06450 |
203-237-4743 |
| Chamberlain Elementary School | 221 Farmington Avenue New Britain, CT 06053 |
860-832-5692 |
| Smith Elementary School | 142 Rutherford Street New Britain, CT 06051 |
860-223-8819 |
| Thomas Jefferson School | 140 Horse Plain Road New Britain, CT 06053 |
860-224-3193 |
| Linden Street School | 69 Linden Street Plainville, CT 06062 |
860-793-6304 x0 |
| Partnership Learning Academy | 77 Main Street Terryville, CT 06786 |
860-516-7002 |
| Regional Behavioral Health Action Organization (RBHAO) overseeing Regional Suicide Advisory Board (RSAB) |
Specific RBHAO town information can be found: https://portal.ct.gov/-/media/DMHAS/Prevention/RBHAOContactspdf.pdf
Specific RSAB town information can be found: https://www.preventsuicidect.org/get-involved/regional-advisory-boards/
| Name | Service Provided | Location | Contact |
| Amplify, Inc. | RBHAO RSAB |
151 New Park Ave, Ste 14A Hartford, CT 06106 |
860-667-6388 |
| Serving: Andover, Avon, Berlin, Bloomfield, Bolton, Bristol, Burlington, Canton, East Granby, East Hartford, East Windsor, Ellington, Enfield, Farmington, Glastonbury, Granby, Hartford, Hebron, Kensington, Manchester, Marlborough, New Britain, Newington, Plainville, Plymouth, Rocky Hill, Simsbury, Somers, South Windsor, Southington, Stafford, Suffield, Tolland, Vernon, West Hartford, Wethersfield, Windsor, Windsor Locks | |||
| Alliance for Prevention and Wellness/A Program of BHcare | RBHAO RSAB |
127 Washington Ave, 3rd Fl North Haven, CT 06473 |
203-736-8566 |
| Serving: Ansonia, Bethany, Branford, Chester, Clinton, Cromwell, Deep River, Derby, Durham, East Haddam, East Hampton, East Haven, Essex, Guilford, Haddam, Hamden, Killingworth, Lyme, Madison, Meriden, Middlefield, Middletown, Milford, New Haven, North Branford, North Haven, Old Lyme, Old Saybrook, Orange, Portland, Seymour, Shelton, Wallingford, Westbrook, West Haven, Woodbridge | |||
| National Suicide Prevention Lifeline | https://suicidepreventionlifeline.org/ | 1-800-273-8255 | |
| Crisis Text Line | https://www.crisistextline.org/text-us/ | Text CT to 741741 | |
| Statewide Programs |
| Name of Agency | Service Provided | Location | Contact |
| FAVOR, Inc. | Family Advocacy Family Peer Support |
185 Silas Deane Highway Wethersfield, CT 06109 |
860-563-3232 |
| Beacon Health Options | CC/Intensive Care Coordination | 500 Enterprise Drive Rocky Hill, CT 06067 |
877-552-8247 |
Disclaimer: This may not be an exhaustive list of the services available in your area. For additional services, you may reach out to your local children’s behavioral health collaborative listed at www.connectingtocarect.org or contact Infoline 2-1-1 Connecticut at www.211ct.org.





